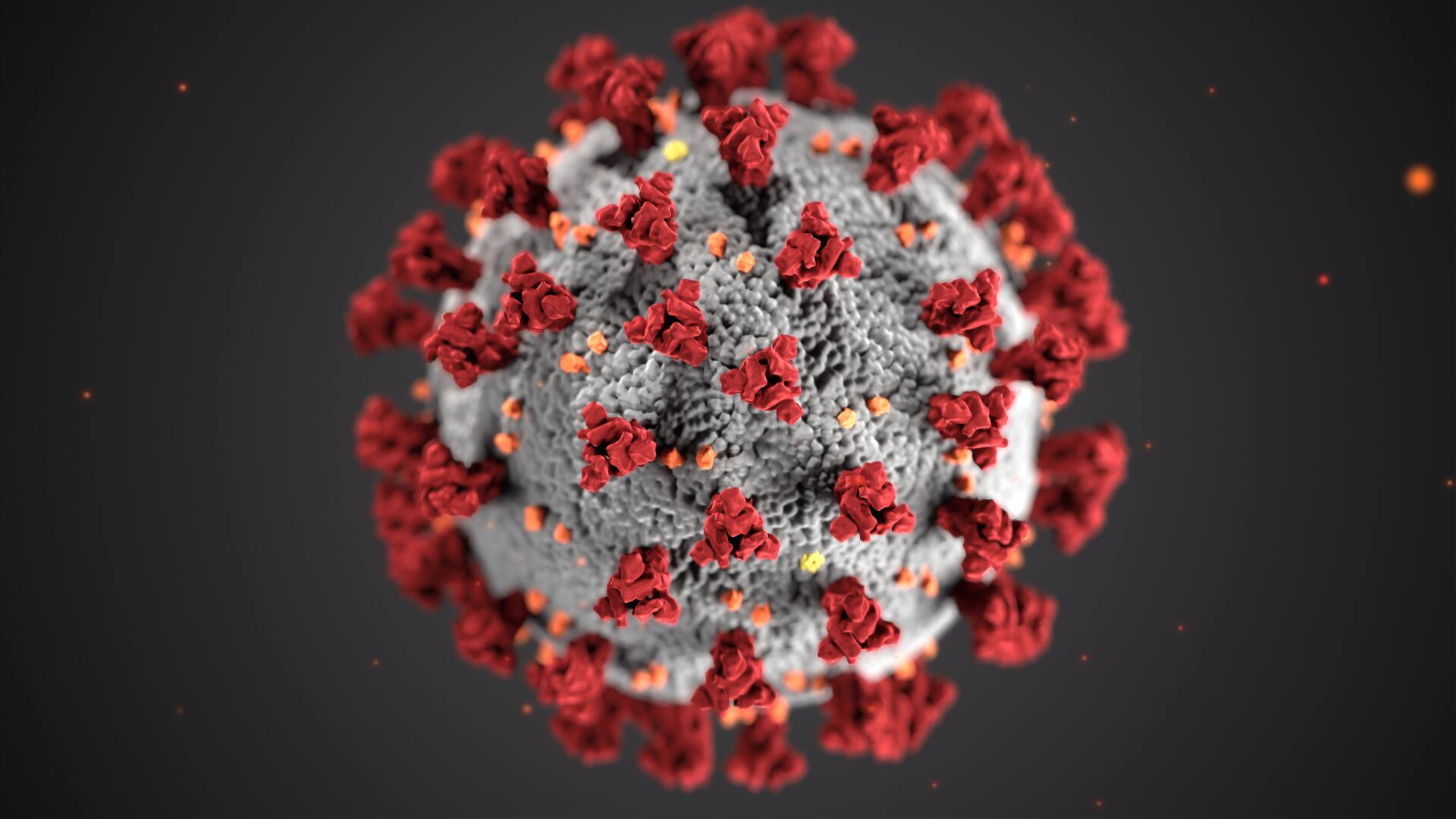
COVID-19 Tests at The Pharmacy at Wellington
Image credit: the Center for Disease Control (CDC)
What are the different COVID-19 tests and which one should I get?
Please keep in mind that COVID-19 is a new disease (it is indeed a novel coronavirus) so information about tests for it is continually evolving. Below is a summary of what is currently known.
Why is testing important?
Early identification of people currently with COVID-19 and people who have had the virus is key for:
- Early monitoring and early treatment to help prevent complications, especially for high-risk individuals;
- Early isolation, to prevent spread;
- Contact tracing so those exposed can self isolate, again to prevent spread;
- Public health officials to understand the prevalence, spread, and contagiousness of the disease, so that mitigation efforts and caseload planning can be more effective; and
- Data gathering by researchers in their efforts to better understand the virus as quickly as possible, in order to develop medicines, vaccines, etc., to save lives.
What kinds of tests are there?
Diagnostic tests available to determine if a person is currently infected:
- Molecular tests
- Also called PCR tests, viral RNA tests, nucleic acid tests
- Antigen tests
- Antigens are substances that cause an immune response in the body. An immune response can be, for example, the production of antibodies.
Tests available to see if a person has been infected in the past:
- Antibody tests
- Also called serologic tests, blood tests
- Antibodies are an immunoglobulin and are made by specialized white blood cells to identify and neutralize foreign substances in the body.
Generally speaking, the true accuracy of COVID-19 tests is unknown due to the following, amongst other possible reasons:
- False negatives and false positives can occur.
- How carefully a specimen is collected and stored may affect accuracy.
- The Federal Drug Agency (FDA) has granted emergency use authorization for COVID-19 testing, which means that the usual vigorous testing and vetting hasn't necessarily taken place as it would ordinarily.
- A large and growing number of companies and laboratories offer COVID-19 tests so accuracy may vary.
- These tests are new and without a long track record; assessments of accuracy can only be approximate.
However, when tests are used to screen for a disease, two measures are used to determine how valid a test is: sensitivity and specificity.
- Sensitivity is the ability of a test to correctly identify patients with a disease.
- Specificity is the ability of a test to correctly identify patients without the disease.
Here's an illustrative example (scroll to the right to see all 5 columns of this table):
| Test XYZ | ||||
|---|---|---|---|---|
| Sensitivity | to identify people with the disease | 90% | 90% of those who have the disease are identified correctly. | 10% of those who have the disease are not detected = false negative |
| Specificity | to identify people without the disease | 80% | 80% of those who don't have the disease are identified correctly. | 20% of those who don't have the disease are misidentified = false positive |
Image credit: Mufid Majnun on Unsplash
Molecular or PCR Tests
How is the test done?
Fluid is collected using a nasal swab, throat swab, or from saliva.
How long does it take to get results?
If analyzed on-site, results can be obtained within minutes, but generally samples are shipped to a laboratory and results take several days.
What does the test look for?
Viral RNA, or the genetic material of the SARS-CoV-2 virus, using a technique called polymerase chain reaction (PCR).
How about accuracy?
Often referred to as the "gold-standard" test, molecular tests are currently more accurate than antigen tests. However, molecular tests are also more expensive than antigen tests. Molecular tests typically do not need to be repeated for accuracy.
Antigen Tests
How is the test done?
Fluid is collected using a nasal or throat swab.
How long does it take to get results?
Results are usually available within 15 minutes to an hour.
What does the test look for?
The presence of certain proteins on the surface of the virus, present in the fluid sample collected.
How about accuracy?
Positive results are considered very accurate. However, there is an increased chance of false-negative results — meaning it is possible to be infected with the virus but have a negative result. The recommended timing for getting an antigen test is at the onset of symptoms (when the virus is actively replicating), or 5 days after the date of exposure to a COVID-19 positive patient (see below, "who should get a diagnostic test?"). Depending on the situation, a molecular test may be recommended to confirm a negative antigen test result.
Who should get a diagnostic test?
A) If you develop any symptoms of COVID-19, even if they are mild, you should get tested. Symptoms may appear 2-14 days after exposure to the virus and may include:
- Fever, chills, or shaking chills
- Signs of lower respiratory illness (cough, shortness of breath, lowered oxygen saturation)
- Fatigue, sore throat, headache, body aches/myalgia, or new loss of sense of taste or smell
- Other less common symptoms can include gastrointestinal symptoms (nausea, vomiting, diarrhea), rash, and inflammatory conditions such as "COVID toes".
OR
B) If you are a close contact of someone who is symptomatic or who has tested positive for COVID-19:
- If you were within 6 feet of them for at least 10-15 minutes, while they were symptomatic or within the 48 hours before symptom onset, OR
- If you were within 6 feet for at least 10-15 minutes of someone who tested positive in the 48 hours before their test was taken or anytime in the 10 days after their test.
If either scenarios A) or B) apply to you, it would be prudent for you to consider getting a diagnostic test.
Antibody Tests
How is the test done?
Finger stick or blood draw.
How long does it take to get results?
Results may be known the same day or within 3 days.
What does the test look for?
The presence of antibodies. To note, it generally takes one to two weeks for our bodies to produce antibodies after an infection, so getting an antibody test too soon may result in a false negative. There is also currently no evidence that a positive antibody test means that a person is immune from COVID-19.
How about accuracy?
Accuracy depends on the presence of antibodies, which may depend on the strength of a person's antibody response, which in turn is dependant upon age, nutritional status, severity of the disease, medications, etc. Sometimes a second antibody test is needed for accurate results.
References and Resources:
- American Heart Association - why testing is important: https://www.heart.org/en/news/2020/04/02/covid-19-science-why-testing-is-so-important
- FDA - types of COVID-19 tests: https://www.fda.gov/consumers/consumer-updates/coronavirus-testing-basics
- CDC - antigen tests: https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antigen-tests-guidelines.html
- Harvard Health - types of testing: https://www.health.harvard.edu/blog/which-test-is-best-for-covid-19-2020081020734
- Government of MA on who should get tested: https://www.mass.gov/covid-19-testing
- CDC - the differences between the flu and COVID-19: https://www.cdc.gov/flu/symptoms/flu-vs-covid19.htm
- CDC - influenza, a prevention timeline: https://www.cdc.gov/flu/pandemic-resources/pandemic-timeline-1930-and-beyond.htm
- Mayo Clinic - what to expect from a nasal swab procedure: https://www.mayoclinic.org/tests-procedures/covid-19-diagnostic-test/about/pac-20488900#:~:text=COVID%2D19%20diagnostic%20testing,19%20%E2%80%94%20molecular%20and%20antigen
- Nature - what rapid antigen tests can and can't do - https://www.nature.com/articles/d41586-020-02661-2
- South Carolina Dept of Health and Environmental Control - symptoms worksheet - https://scdhec.gov/sites/default/files/media/document/CDC-Flyer-14-Day-Monitoring-Worksheet-10.20.2020.pdf
- Arkansas Department of Health - what is antibody testing - https://www.healthy.arkansas.gov/images/uploads/pdf/Antibody_Testing_(1).pdf
- Chemial & Engineering News, American Chemical Society - how the Quidel Sofia 2 SARS Antigen Test works - https://cen.acs.org/analytical-chemistry/diagnostics/COVID-19-antigen-tests-landed/98/web/2020/06
- BMJ Journal, Evidence-Based Nursing - sensitivity and specificity: https://ebn.bmj.com/content/23/1/2
- BMJ Journal, Covid-19 laeral flow tests: https://www.bmj.com/content/371/bmj.m4469#